Eric Garland, associate dean for research in the College of Social Work at the U, was recently awarded two multi-million dollar grants from the National Institutes of Health and the Department of Defense.
For over 22 years, Garland has personally practiced mindfulness — a practice of focusing “attention to the present moment experience” rather than the past or future “as a way to expand awareness.” He experienced its value in “strengthening well-being and resilience” firsthand.
Garland began studying mindfulness as a treatment for alcoholism during his fellowship in integrative medicine at the University of North Carolina at Chapel Hill. After moving to Salt Lake City, he decided to follow up on his research and pursued funding for new studies.
The grants Garland received will help take his research in a new direction — opioid-related problems.
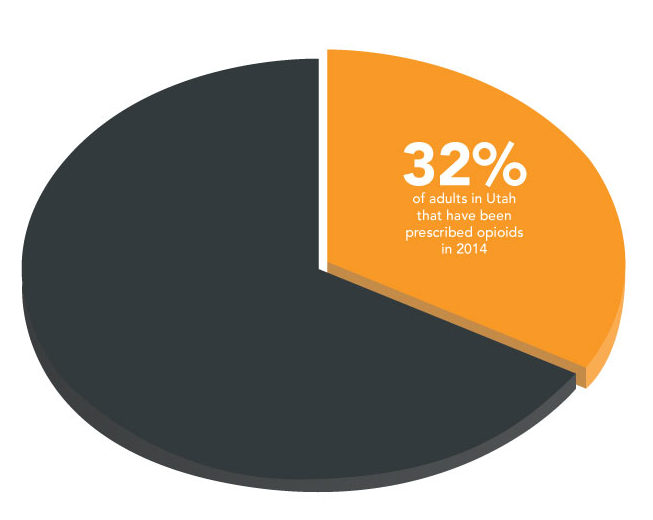
Opioids are medications that work in two ways: they relieve pain by reducing the intensity of the signal going to the brain and they change the brain itself to lessen the effects of pain. These drugs are powerful and often prescribed for chronic pain, but over time they may “not give as much relief as the person needs,” Garland said. A press release from the U announcing the grants says that the gap in pain relief combined with the way chronic opioid use changes the brain can lead to problems such as elevated pain sensitivity, reduced responsiveness to feelings of pleasure and vulnerability to risky use such as dose escalation.
Garland’s grants will fund two studies — one to see if a treatment called Mindfulness-Oriented Recovery Enhancement (MORE) will help veterans and military personnel who are prescribed opioids, and a second to evaluate the effects of MORE on endorphin levels and whether or not this explains changes in chronic pain.
MORE uses three therapeutic techniques — mindfulness, reappraisal and savoring. These “mental training techniques” encourage patients to focus on the present moment, cope with stress and negative emotions and restore sensitivity to natural, healthy pleasures for a greater sense of happiness and well-being.
The research is designed to fill significant gaps in academic knowledge. Garland says a lot is known about use of illicit opioids like heroin, but not as much about how long-term use of prescription opioids affects the brains of chronic pain patients. According to Garland, historically there was a “belief in the medical system that taking opioids for pain would not result in brain changes that increase vulnerability to risky opioid use.” Medical experts now know that this isn’t the case.
While Garland’s research focuses on providing treatment to chronic pain patients who have long-term opioid prescriptions, but he also has ideas for preventing riskly opioid use and other related problems at the outset. He feels intervention needs to take place before acute pain develops into chronic pain. At that point, Garland believes doctors should offer prescription medications in addition to psychological therapies like MORE and physical therapies like exercise training. Garland advocates “meditation along with medication.”
@EliseAbril