Buening: Birth Control Isn’t a Cure-All
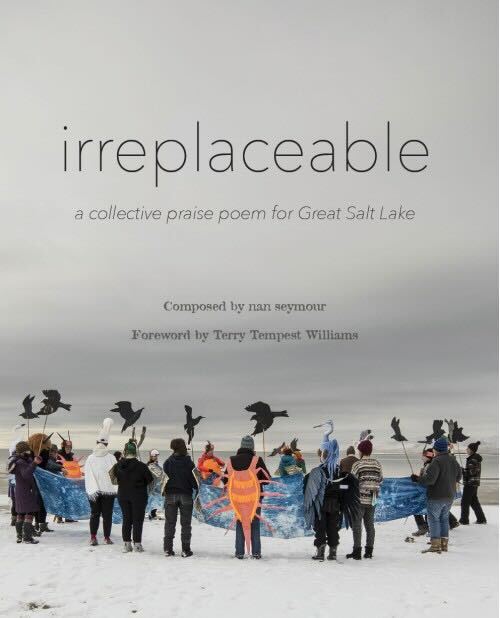
Emergency contraceptive with security protections at Smith’s Food and Drug in Salt Lake City, on Tuesday, November 2, 2021 (Photo by Brooklyn Critchley | The Daily Utah Chronicle)
November 5, 2021
As a teenager experiencing painful, unmanageable periods, I mentioned my discomfort to my doctor. After that, my doctor didn’t hesitate to prescribe hormonal birth control pills. Beforehand, my dermatologist had recommended the pill as a way to manage acne. So, I thought I might as well take the pill.
But after a few months, I began feeling increasingly tired and irritable. I even started developing acne flare-ups, despite my dermatologist’s recommendation. At that point, I was told that different types of birth control can negatively impact your skin. Confused and frustrated, I stopped taking it.
Menstrual cycles vary greatly from person to person. Regularity, flow, color, cramping and PMS symptoms depend on complicated genetic and lifestyle factors. It makes sense that people experience varied reactions to contraceptive pills. But most menstrual issues get lumped into a generic category with birth control as the one common treatment.
Hormonal birth control is not a cure-all for women’s health issues. While contraception should certainly be accessible, women need the ability to make informed decisions about their health. Our perspective of menstrual treatments needs to expand beyond the pill.
Women have unique health concerns regarding menstrual cycles. Irregular or absent periods can indicate larger health concerns ranging from vitamin deficiencies to disease. Activity levels and dietary habits have a large influence on degrees of period pain. Hormone fluctuations around menstruation also impact mood and can cause breakouts.
This only demonstrates a snapshot of a period’s various implications. For such a diverse set of symptoms and causes, we should have an equally diverse set of approaches. But many times, bringing up any of these concerns lands people the same birth control prescription I got as a cramping teenager.
These hormonal pills certainly have their uses. I oppose efforts to restrict contraceptive access. Birth control options are important in preventing unwanted pregnancies and in the right circumstances, addressing some of the aforementioned health issues.
Women should have the right to access and choose hormonal contraception as an option. But we shouldn’t treat it as the only option.
I personally know many women who had similar experiences to mine on different forms of contraceptive, particularly hormonal forms. One Crisis Magazine article shared the experiences of several young women who were prescribed birth control to treat anything and everything. One woman’s doctor said, “Prescribing the pill for your condition is like killing a flea with an elephant gun.”
Most women will use contraceptives at some point during their lifetime. Those that use hormonal birth control will often experience these types of negative impacts. For many, their underlying issues don’t require such strong medicine. If anything, they are dangerous.
Hormonal birth control, like any medication, can impact us in unpredictable ways. One Denmark study analyzed data from national health information systems. It concluded that hormonal contraception carries an increased risk of developing depression, especially among teenagers.
Other common side effects of hormonal birth control include weight gain, lowered libido, heightened risk of blood clots, mood changes and nausea. While some of these effects are already natural responses during periods, they worsen with birth control. Depending on the person, they can exacerbate pre-existing conditions.
By prescribing birth control to nearly every women’s health concern, we also ignore underlying health causes. For example, women with severe endometriosis can receive a birth control prescription where they actually need surgery to remove diseased uterus tissue. In cases like these, prolonging the treatment of underlying causes can lead to issues like infertility. Periods are powerful indicators of bodily health. We can’t afford to ignore our bodily cues by repressing them with medicine we don’t always need.
To better address menstrual health issues and avoid these negative health impacts, we need to do what cycle nutritionist Nicole Bendayan calls “connecting with our feminine cycles.” As her site teaches, we need to take more holistic approaches to optimize our health and wellness. In other words, we need better education about menstrual processes.
Bendayan is a much-needed leader in spreading feminine health awareness. Upon visiting her site, I was surprised to learn how oral contraceptives deplete some of our essential nutrients, harm good bacteria and pose the risk of post control syndrome. I wish I knew about these consequences before I began taking birth control. I wish I had been told about alternative solutions.
Treating birth control as a “cure-all” improperly addresses our health challenges. Changing the way we treat women’s health issues is necessary to achieve better wellness. Oftentimes, changing aspects of our lifestyles can yield more results better for our health than prescribing pills at the drop of a hat. We need to recognize that birth control can be a powerful tool for women when implemented correctly. Otherwise, it can do more harm than good.