Like any organ, doctors occasionally need to examine the inside of a patient’s brain to see the cells. The most common ways to do this currently are: cutting out a section of the brain and observing it under a microscope or inserting an optical probe inside the brain.
A group of U researchers from diverse disciplines—genetics, neurobiology and engineering—recently created a new way to image the inside of a brain with less damage. It causes less injury because the invasion is much smaller. It is made with a glass surgical needle and it measures 220 micrometers in diameter, not much larger than a single strand of hair and much smaller than any other type of probe used today.
The brain is an exceptionally delicate organ. This can be seen clearly in a video produced by the University of Utah Neuroscience Initiative featuring Dr. Suzanne Stensaas, a Professor of Neurobiology and Anatomy at the medical school, and a recently autopsied human brain (warning: this video is graphic). Just by holding the brain, Stensaas damages it.
Since the brain is so fragile, both probing and biopsy can be damaging to the important tissue. For example, risk factors for brain biopsy include hemorrhaging or hydrocephalus, a condition where fluid builds up in the brain. It causes symptoms like headaches, vomiting, nausea, blurred or double vision, balance and coordination problems, urinary incontinence, drowsiness, memory loss and personality changes. Scarring after these procedures can also cause seizures.
The new imaging technique uses a very small glass needle, and researchers believe this drastically reduces the possibility of damage. The study says, “no structural deformation is expected during imaging or implantation.”
Rajesh Menon, one of the researchers and Assistant Professor of Electrical and Computer Engineering, explains the process. The needle, called a cannula, acts as a conduit for light sent through it into the brain where cells are illuminated. The cannula also collects the light signal from the cells and carries it back outside the brain, “where it is recorded on an image sensor,” according to Menon. As light reenters the cannula, if it’s angled at all, it bounces back and forth inside the needle creating multiple reflections and scrambling the image of the cells. Menon says, “We developed algorithms to unscramble this image and produce a high-resolution image that is familiar to neuroscientists.”
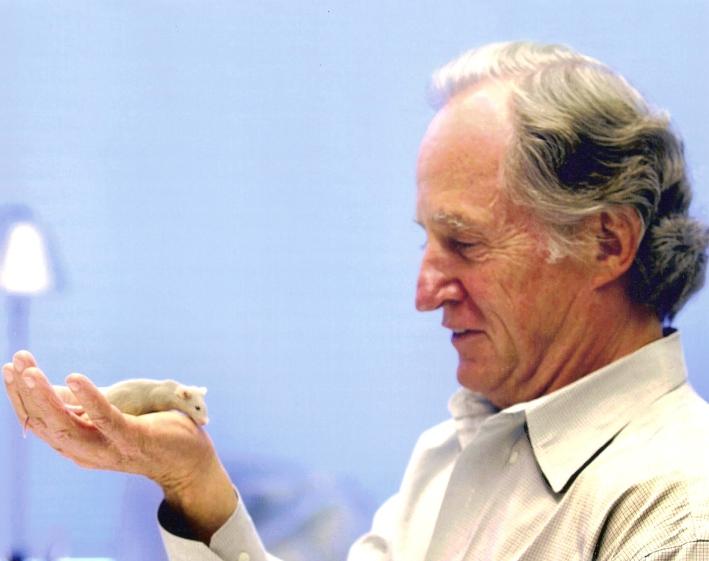
The team tried the technique in mice, which had been genetically engineered in U Nobel Laureate Mario Capecchi’s lab to make certain brain cells fluorescently glow when lit up. Capecchi’s lab donated the mice, as well as helped the team design the imaging technique and interpret the results of the tests.
On the diversity in the specialty of their research team, Menon says, “In my experience, a majority of innovation happens at the intersections of seemingly wildly different fields and this is one such example. Scientists with different backgrounds, not only have different training but different intuition and ways to look at the same problem. Such different points of view, which can also arise from increased diversity in race and gender, gives rise to unique and effective solutions.”
The new method created by the diverse team has implications for deep brain imaging, which can be riskier because it offers more possibility for damage.
Menon says they anticipate to explicitly measure the damage caused by their technique soon. This will allow them to more accurately compare it to other methods of imaging.
The team hopes that eventually the technique can be used in humans.
@EliseAbril